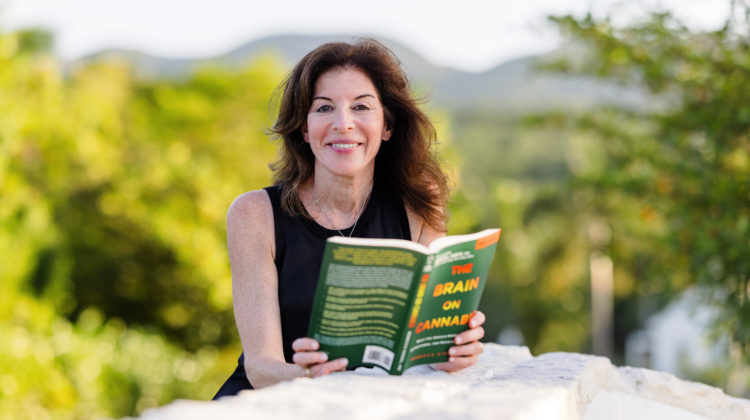
Photo contributed by: Beth Graham
Opioids have been the standard for managing both chronic and short-term pain for a long time. While they have their place in medicine, they definitely have their drawbacks.
The CDC estimates that 75,673 Americans died from opioid overdoses between April 2020 to April 2021. Aside from the risk of overdose, opioids are highly addictive and can cause heart problems and weaken bones, according to the CDC.
As a result of such concerns, the CDC recently released new guidelines for opioid prescriptions. They also suggested alternative treatment options.
“I think the CDC’s changing recommendations is a huge thing and a move forward in that they really want to recommend that doctors turn to the non-opioid type therapies,” said Dr. Rebecca Siegel. Siegel is a physician in New York and author of The Brain on Cannabis: What You Should Know About Recreational and Medical Marijuana.
The new set of guidelines advises physicians to limit new opioid prescriptions and recommend alternate treatment methods. These guidelines apply to the treatment of short-term pain, pain lasting from one to three months and chronic pain.
Post from @drrebeccasiegel on Instagram.
Using Cannabis to Manage Pain
The CDC did not list cannabis as an alternative treatment option. However, there is evidence that suggests medical cannabis can help to manage chronic pain and reduce opioid use.
A study, published in July of 2020, found a 64% to 75% reduction in opioid use when used in conjunction with medical cannabis. The 7,222 study participants all experienced non-cancer related chronic pain.
“There is some available evidence for the effectiveness of cannabis-based medicine for certain types of chronic pain, but cannabis is not a one size fits all drug. For some it may be helpful, for others absolutely not,” Siegel told Emerald.
Patients can use medical cannabis to manage symptoms of conditions. Some of these conditions include insomnia, chronic back pain, cancer and Post Traumatic Stress Disorder (PTSD), according to Siegel. This also included management of neuropathic pain for things like Multiple Sclerosis (MS), Lupus, Irritable Bowel Syndrome (IBS) and Crohn’s Disease.
Siegel always recommends her patients consume medical cannabis in the forms of a capsule, tincture or edible. This limits negative effects on the lungs that come with smoking or vaping cannabis.
There are multiple reasons why physicians and the CDC are hesitant to recommend medical cannabis as a treatment option, Siegel said. Some of these reasons are: the stigma associated with cannabis, federal law, lack of sufficient research and lack of awareness.
Experts do not agree on whether cannabis can be addictive and dependence forming when used to manage medical conditions.
“Cannabis may be addictive for some and may be dependence forming for some. We know that opioids are definitely abusable and dependence forming very quickly,” Siegel added. “Cannabis is more of a complicated issue and there is no real consensus.”
A Physician’s Point of View
Medical schools do not provide education or training regarding the prescription of medical cannabis to treat certain conditions.
Siegel admits that she lacked awareness, education and understanding about how medical cannabis can be utilized to help her patients.
Siegel credits her newfound knowledge of medical cannabis to a woman she called “patient zero.”
Post from @drrebeccasiegel on Instagram.
Patient zero struggled with insomnia, and after a trip to Colorado, found something that helped her. She went to Dr. Siegel and told her that an edible cured her insomnia. But she needed a more sustainable way to access cannabis in her home state of New York.
After researching medical cannabis, Siegel was then able to provide patient zero with a medical cannabis certification.
Patient zero eventually inspired Siegel to write her book The Brain on Cannabis.
“I am definitely not one who is pushing anybody to use cannabis for any type of treatment […]. But if I was so clueless, many others might be as clueless or more clueless about how it might help or how it might hurt,” Siegel said.
The History and Future of Medical Cannabis
Anthropologists estimate that cannabis was first used medicinally around 400 AD. Even in the U.S., medicinal use of cannabis dates back to the 19th century. This ended with the passage of the Marihuana Tax Act of 1937, according to a study published in the Journal of Pharmacy and Therapeutics.
Restrictions on cannabis use only increased with the passage of The Boggs and Narcotic Acts, and the Controlled Substances Act (CSA). The CSA identifies cannabis as a schedule I substance.
This status means cannabis has no officially recognized medical value. Additionally, it prevents researchers from studying it.
This explains why cannabis research is insufficient and far behind other medicinal treatments when it comes to managing medical conditions.
But, as the opioid epidemic continues, the medical community has begun to seek out alternatives, according to the Journal of Pharmacy and Therapeutics study. Medical cannabis is one alternative. However, there is still some hesitancy.
“If cannabis is ever going to be thought of as a real medication that physicians will recommend to patients, there has to be a standardized product and there also has to be some sort of federal guideline,” Siegel explained.
Why Seek Medical Cannabis When Recreational Cannabis is Available?
As more states legalize recreational cannabis, the appeal of medical cannabis decreases, Siegel said.
“The medical use of cannabis is trying to catch up with adult use, because if everyone is going to turn to adult-use dispensaries when they’re 21, why use medical?” Siegel said.
Consequently, Siegel suggested that the best way to use cannabis to treat medical conditions is to consult a physician. While doctors are becoming increasingly aware of medical cannabis’ benefits, some physicians can provide a medical certification and recommend products.
Furthermore, seeking medical advice allows patients to know what dosage and products will help them, according to Siegel. However, there may not be much difference in the price or quality of medical and recreational cannabis in most states.
Therefore, patients must pay for heavily taxed medical cannabis out of pocket.
“My hope is that there is a real use for medical cannabis and that health insurance companies have to start reimbursing medical cannabis,” Siegel said.


WHOLE PLANT “chemical free” Cannabis, Hemp, and Weed for Patient/public safety = please don’t listen to the while coats 🙂
Currently using cannabis in hospice care for my 44 year young son whom was medically injured at Yale/New Haven in 2009. Horrible experience, misdiagnosed a massive stroke! Yale has a clinic for long term survivor childhood cancer patients.
Now living in medical poverty as I do not get paid to take care of him, even though Yale created his situation.
The white coat criminals.
The AMA is corrupt, medicare is a joke, being disabled in America is hell.
If a doctor does NOT titrate and CANNOT TALK ABOUT personal titration = in other words, the doctor titrates the SAME BOTANICAL INPUTS as we do, then that is NOT a doctor 🙁
Cannabis is what we do with it 🙂
This is EXISTENTIAL MEDICINE so “dosing” is complete QUACKERY if we have more than ZERO and do NOT overdose 🙂
We are SICK AND TIRED of this formatting bec. CANNABIS IS WHAT WE DO WITH IT intellectually eviscerates THIS IDEA that there are EXPERTS who TELL US WHAT TO DO = after THREE YEARS + of people TELLING US WHAT TO DO we ARE SICK AND TIRED of people thinking they can tell us what to do 🙂
Just stop please with this formatting: there are NO EXPERTS in CANNABIS/HEMP/WEED and there won’t be for perhaps 15-20 years; today’s “experts” are FRAUDS 🙂